Inflammatory bowel disease (IBD), including Crohn's disease and ulcerative colitis, is characterized by an activation of the immune system in the digestive tract, the exact cause of which remains unknown to this day (1). Genetic and environmental factors (e.g., smoking, nonsteroidal anti-inflammatory drugs (NSAIDs), diet), gut microbiota, and immune response seem to play a role in its development (1, 2).
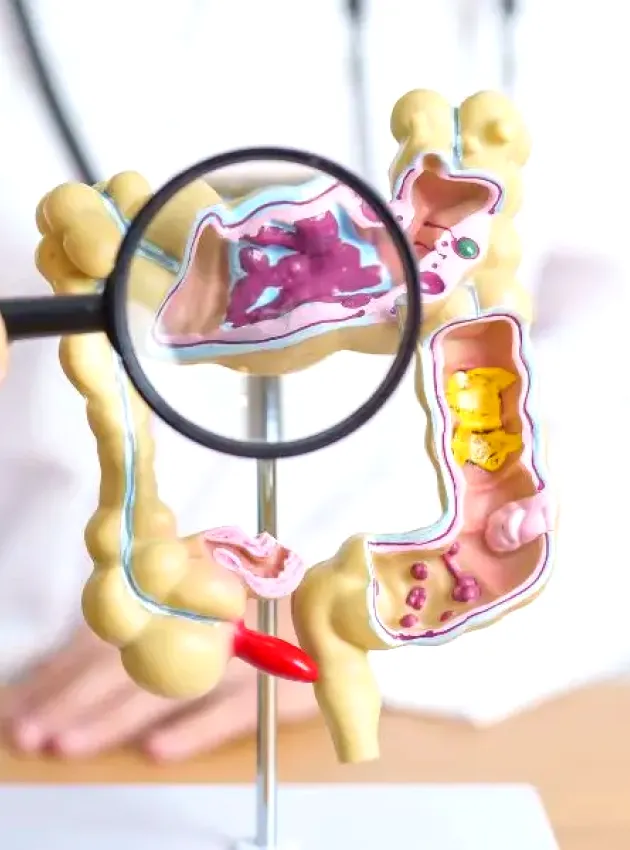
Pathophysiology and complications
Several hypotheses exist to explain the etiology of IBD. The first is an alteration of the intestinal barrier, allowing bacterial fragments to penetrate the intestinal epithelium, triggering a localized chronic inflammatory reaction (2). Additionally, changes in the microbiotic composition, such as a reduction in bacterial diversity and an increase in the abundance of pathogens, as well as the altered function of intestinal microbiota, are often observed (2). For example, in Crohn's disease, these disturbances include a decrease in beneficial bacteria such as Akkermansia muciniphila, Bifidobacteria spp., and F. prausnitzii, and a proliferation of pathogens such as E. coli and Candida tropicalis (2).
The complications associated with IBD depend on the affected region of the intestine. During active phases of Crohn’s disease, symptoms include abdominal pain, diarrhea, weight loss, and fatigue. Complications such as fistulas, stenoses, and mouth ulcers may also occur (4). Ulcerative colitis, in contrast, primarily features mucosal ulcers specifically in the colon and is often characterized by stools containing mucus and blood, as well as an increased frequency of rectal bleeding (5). During acute phases, anal fissures, fistulas, abscesses, and even intestinal obstructions and perforations may occur (5). Living with IBD increases the risk of malnutrition, dehydration, and deficiencies in iron and vitamin D, highlighting the importance of paying close attention to diet quality depending on the phase and symptoms (2). IBD is also associated with other health conditions such as anemia, osteoporosis, and long-term colon cancer risk (5).
Nutritional strategy in the remission phase
Diet plays an integral role in the treatment of patients living with IBD, as it significantly influences the composition and function of the gut microbiota, intestinal barrier, host immunity, and intestinal physiology. Currently, no specific diet is recommended to promote remission or prevent relapses (6). A recent meta-analysis (2023) indicates, with limited evidence (low to very low quality), that low refined carbohydrate diets and symptom-guided exclusion diets may promote remission in people with Crohn's disease (7). The review also shows that specific carbohydrate and Mediterranean diets offer similar benefits, although the Mediterranean diet may be more favourable for adherence. Conversely, interventions that exclude carrageenan and dairy products do not appear to have a significant effect on IBD remission (7). Despite these low-quality conclusions, Mediterranean-style dietary patterns, limiting red and processed meat while increasing intake of fruits, vegetables, and omega-3-rich fish, are strongly recommended by the ESPEN expert group for their anti-inflammatory properties and positive impact on the microbiota (1, 6). A recent clinical study (n=53) compared the effects of an anti-inflammatory diet (characterized by increased intake of antioxidants, dietary fibre, probiotics, omega-3s, and reduced intake of red and processed meat and added sugars) and a control diet (following the principles of Canada’s Food Guide) in participants with ulcerative colitis in remission for six months. The authors found no statistically significant differences regarding relapses, but promising changes were observed in the intervention group, including reduced colonic inflammation measured by fecal calprotectin, as well as positive changes in gut bacterial composition and their metabolites (8). Thus, nutritional recommendations should be personalized and based on an individualized approach, pending more robust, high-quality research to provide solid foundations for more generalized nutritional recommendations.
Dietary fibre: the key to success?
During active phases of IBD, some patients reduce their dietary fibre intake as a nutritional therapy to alleviate symptoms. However, contrary to some beliefs, patients without intestinal strictures do not need to limit their fibre intake outside of flare-up periods. Dietary fibre is essential for supporting the diversity and health of gut flora. A fibre-rich diet (at least 30 g per day) and prebiotics (found in many plants like chicory root, garlic, onion, wheat bran, and raw bananas) are recommended throughout the remission phase (6, 9). A dietitian-nutritionist as part of the multidisciplinary team is essential to guide your patients in reintegrating, increasing, and gradually diversifying fibre intake (6, 9).
Future avenues: emulsifiers, pesticides, and probiotics
Certain emulsifiers, herbicides, and probiotics are also avenues to explore. Emulsifiers are substances that help mix two immiscible liquids, such as oil and water, and are commonly used in food products to improve texture, extend shelf life, and enhance consistency. However, their impact on health, particularly for those with IBD, is subject to ongoing research. Experimental studies and now a clinical study suggest that the emulsifier carboxymethylcellulose may contribute to negative changes in the microbiota (6, 10). These preliminary findings show that a diet rich in whole, unprocessed foods, which are less likely to contain emulsifiers, should be favoured to limit risks.
Exposure to certain pesticides, notably glyphosate, the most widely used herbicide in America, can alter intestinal permeability and disrupt the microbiota, potentially contributing to the development of IBD (11). For some plant-based products, it may be advantageous to choose organic versions, especially when they are likely to contain high concentrations of glyphosate and other pesticides (e.g., oats and corn).
Regarding probiotics, they are not currently recommended for the treatment or prevention of active IBD or recurrences (6). However, some studies suggest that specific probiotic strains may help reduce flare-ups and IBD symptoms. In a randomized, multicenter, controlled clinical trial, patients who consumed the VSL#3 formula twice a day for 12 weeks showed significantly higher remission rates compared to the placebo group (43% vs. 16%). Additionally, Disease Activity Index scores for ulcerative colitis decreased by 50% (12). A small study also showed a reduction in clinical relapse rates after six months of S. boulardii use compared to a placebo in participants living with Crohn’s disease (13). Despite these promising results, expert committees cannot yet draw firm conclusions due to several other clinical studies reporting no effect (6). In general, probiotics are considered safe, with few side effects. Including food sources of probiotics like kefir, tempeh, miso, and sauerkraut, as well as supplements when necessary, could be an integral part of nutritional support with a professional.
There is no definitive cure for inflammatory bowel diseases (except surgery in some cases), but a nutritional approach can help manage symptoms and prevent future flare-ups. At TeamNutrition, we offer personalized support to optimize digestive health and minimize IBD complications. To find out how our dietitians can assist you, visit our website or contact us directly.
References
- Reznikov, E. A., & Suskind, D. L. (2023). Current nutritional therapies in inflammatory bowel disease: improving clinical remission rates and sustainability of long-term dietary therapies. Nutrients, 15(3), 668.
- Société savante des malades et cancers de l'appareil digestif. (2018) Maladie de crohn. Retrieved from https://www.snfge.org/content/maladi e-de-crohn-0#:~:text=Le%20 diagnostic%20de%20maladie%20de,la%20muqueuse%20intestinale%2C%20typiquement%20des
- Pascal, V., Pozuelo, M., Borruel, N., Casellas, F., Campos, D., Santiago, A., ... & Manichanh, C. (2017). A microbial signature for Crohn's disease. Gut, 66(5), 813-822.
- Leyla J Ghazi, M. (2019). Crohn disease differential diagnoses. Retrieved from https://emedicine.medscape.com/article/172940-differential
- Cleveland Clinic. (2023). Ulcerative Colitis. Retrieved from https://my.clevelandclinic.org/health/diseases/10351-ulcerative-colitis
- Bischoff, S. C., Bager, P., Escher, J., Forbes, A., Hébuterne, X., Hvas, C. L., ... & Weimann, A. (2023). ESPEN guideline on Clinical Nutrition in inflammatory bowel disease. Clinical Nutrition, 42(3), 352-379
- Limketkai, B. N., Godoy-Brewer, G., Parian, A. M., Noorian, S., Krishna, M., Shah, N. D., White, J., & Mullin, G. E. (2023). Dietary Interventions for the Treatment of Inflammatory Bowel Diseases: An Updated Systematic Review and Meta-analysis. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association, 21(10), 2508–2525.e10.
- Keshteli AH, Valcheva R, Nickurak C, et al. Anti-inflammatory diet prevents subclinical colonic inflammation and alters metabolomic profile of ulcerative colitis patients in clinical remission. Nutrients 2022;14:3294.
- Crohn et colite Canada. (n.d.). Régime et nutrition. Retrieved from https://crohnetcolite.ca/A-propos-de-ces-maladies/Parcours-de-la-MII/Regime-et-nutrition
- Chassaing, B., Compher, C., Bonhomme, B., Liu, Q., Tian, Y., Walters, W., ... & Lewis, J. D. (2022). Randomized controlled-feeding study of dietary emulsifier carboxymethylcellulose reveals detrimental impacts on the gut microbiota and metabolome. Gastroenterology, 162(3), 743-756.
- Chen, X., Wang, S., Mao, X., Xiang, X., Ye, S., Chen, J., ... & Wang, X. (2023). Adverse health effects of emerging contaminants on inflammatory bowel disease. Frontiers in Public Health, 11, 1140786.
- Sood, A., Midha, V., Makharia, G. K., Ahuja, V., Singal, D., Goswami, P., & Tandon, R. K. (2009). The probiotic preparation, VSL# 3 induces remission in patients with mild-to-moderately active ulcerative colitis. Clinical gastroenterology and hepatology, 7(11), 1202-1209.
- Guslandi, M., Mezzi, G., Sorghi, M., & Testoni, P. A. (2000). Saccharomyces boulardii in maintenance treatment of Crohn’s disease. Digestive diseases and sciences, 45, 1462-1464.