In Canada, thyroid disorders affect about 1 in 10 adults, with women being up to eight times more affected than men (1,2). Hashimoto’s thyroiditis is the most common cause of hypothyroidism in Western countries (3,4).
Autoimmune conditions: the main cause of thyroid disorders
Hashimoto’s thyroiditis results from an immune system dysfunction involving a genetic predisposition as well as environmental factors such as (5):
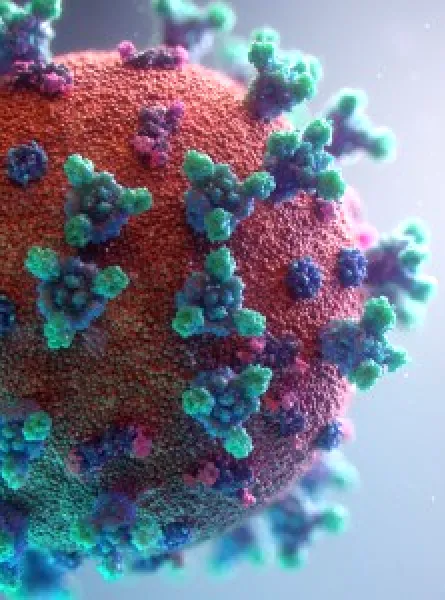
- Viral infections
- Oxidative stress
- Radiation exposure
- Gut dysbiosis
Or micronutrient imbalances, including:
- Selenium deficiency
- Vitamin D deficiency
- Excessive iodine intake
Metabolic and systemic consequences of hypothyroidism
Complications associated with untreated hypothyroidism (including Hashimoto’s thyroiditis) go beyond the classic symptoms. They may include:
- An increased risk of cardiovascular disease and dyslipidemia (6,7)
- Insulin resistance, observed in people living with Hashimoto’s (8)
- Iron-deficiency anemia, which is common in this context (9)
Chronic inflammation appears to play a central role by promoting both insulin resistance and increased production of hepcidin, a hormone that blocks intestinal iron absorption (8,9).
In this context, registered dietitians can help identify, prevent, and manage metabolic complications associated with hypothyroidism, notably by optimizing the intake of key nutrients for thyroid function and by modulating chronic inflammation through targeted nutritional interventions.
The key role of dietitians in managing thyroid disorders
Treatments such as levothyroxine are essential, but their effectiveness depends on proper adherence, management of food interactions (e.g., calcium, coffee), and careful monitoring of nutrient deficiencies. This makes support from registered dietitians indispensable in the management of thyroid disorders.
Key micronutrients in thyroid physiology
|
Nutrient |
Role in thyroid function / Hashimoto’s |
Main dietary sources |
Recommendations / Precautions |
|---|---|---|---|
|
Iodine (10) |
Essential for thyroid hormone synthesis; deficiency or excessive intake can worsen hypothyroidism. |
Iodized salt, milk, cheese, seafood (e.g., fish, shrimp), seaweed |
Recommended intake: 150 μg/day (equivalent to 250 mL of milk and ¼ tsp iodized salt). |
|
Selenium (11) |
Cofactor for the enzyme that converts T4 (inactive) to T3 (active); supplementation may reduce serum thyroid antibody levels. |
Brazil nuts, fish, meat, eggs |
Optimal intake: 100–200 μg/day (about 2–4 Brazil nuts). |
|
Zinc (12) |
Contributes to the synthesis and action of thyroid hormones. |
Seafood, meat, nuts, seeds |
Prioritize dietary intake. |
|
Iron (5, 9) |
Bidirectional relationship; deficiency can worsen thyroid disorders and thyroiditis can impair iron absorption. |
Red meat, poultry, fish, eggs, pumpkin seeds, tofu, leafy greens |
Supplementation is necessary if deficient. |
|
Vitamin D (13, 14) |
Deficiency is linked to more severe forms of Hashimoto’s; supplementation may improve TSH levels and reduce serum thyroid antibody levels. |
Fatty fish, eggs |
Supplementation is recommended. |
|
Gut microbiota (15) |
Influences the absorption of certain nutrients (iron, iodine, selenium, zinc) and can worsen inflammation if imbalanced. |
Fibre, fermented foods, a plant-rich and diverse diet |
Modulating the gut microbiota is a promising avenue for managing Hashimoto’s thyroiditis. |
Modulating inflammation through the gut microbiota
The gut–thyroid axis is of growing interest in understanding Hashimoto’s thyroiditis. Gut dysbiosis may worsen hypothyroid symptoms by:
- Weakening the intestinal barrier
- Activating pro-inflammatory immune responses
- Impairing the absorption of nutrients essential to thyroid function, such as iron, iodine, selenium, and zinc (15)
Patients often show a reduced production of short-chain fatty acids, key metabolites for inflammation regulation (15).
Although clinical data on the direct impact of microbiota modulation on thyroid function remain limited, certain dietary habits appear promising:
- Eat a varied diet (ideally ~30 different plants per week)
- Consume adequate fibre (30 to 50 g/day)
- Include fermented foods (natural probiotic sources)
Such an eating pattern is a promising strategy to strengthen the gut microbiota and support immune health.
Personalized nutritional support for thyroid health
Given the complexity of thyroid disorders and the involvement of multiple nutritional factors, a multidisciplinary approach is essential. The registered dietitians at ÉquipeNutrition are qualified to:
- Assess nutritional intake
- Correct deficiencies
- Implement evidence-based, personalized interventions
- Support thyroid health and help reduce associated complications
Make it easier for your patients to access complementary care alongside medical treatment with our registered dietitian consultations. Visit our medical referral page to learn how to refer your patients and access the referral form.
References
- ThyForLife. (2023). Prevalence of thyroid diseases. https://www.thyforlife.com/prevalence-of-thyroid-diseases/
- Cleveland Clinic. (2023). Thyroid disease. https://my.clevelandclinic.org/health/diseases/8541-thyroid-disease
- Anandkumar, S., Chacko, J., Theertha, C. K., & Usha, M. (2020). Thyroid Disorder: An Overview. Research Journal of Pharmacology and Pharmacodynamics.
- Walsh, J. (2016). Managing thyroid disease in general practice. Medical Journal of Australia, 205.
- Mikulska, A. A., et al. (2022). Metabolic Characteristics of Hashimoto’s Thyroiditis Patients and the Role of Microelements and Diet in the Disease Management—An Overview. Int. J. Mol. Sci., 23, 6580.
- Rodondi, N., et al. (2010). Subclinical hypothyroidism and the risk of coronary heart disease and mortality. JAMA, 304(12), 1365–1374.
- Cappola, A. R., Desai, A. S., Medici, M., Cooper, L. S., Egan, D., Sopko, G., ... & Ladenson, P. W. (2019). Thyroid and cardiovascular disease: research agenda for enhancing knowledge, prevention, and treatment. Circulation, 139(25), 2892-2909.
- Lei, Y., Yang, J., Li, H., Zhong, H., & Wan, Q. (2019). Changes in glucose‐lipid metabolism, insulin resistance, and inflammatory factors in patients with autoimmune thyroid disease. Journal of clinical laboratory analysis, 33(7), e22929.
- Garofalo, V., et al. (2023). Relationship between Iron Deficiency and Thyroid Function: A Systematic Review and Meta-Analysis. Nutrients, 15(22), 4790.
- National Institutes of Health, Office of Dietary Supplements. (2022, March 29). Iodine: Fact sheet for health professionals. https://ods.od.nih.gov/factsheets/Iodine-HealthProfessional/
- Wichman, J., Winther, K. H., Bonnema, S. J., & Hegedüs, L. (2016). Selenium supplementation significantly reduces thyroid autoantibody levels in patients with chronic autoimmune thyroiditis: a systematic review and meta-analysis. Thyroid, 26(12), 1681-1692.
- Walker, C. F., Kordas, K., Stoltzfus, R. J., & Black, R. E. (2005). Interactive effects of iron and zinc on biochemical and functional outcomes in supplementation trials. The American journal of clinical nutrition, 82(1), 5-12.
- Talaei, A., Ghorbani, F., & Asemi, Z. (2018). The effects of vitamin D supplementation on thyroid function in hypothyroid patients: a randomized, double-blind, placebo-controlled trial. Indian journal of endocrinology and metabolism, 22(5), 584-588.
- Durá-Travé, T., & Gallinas-Victoriano, F. (2024). Autoimmune Thyroiditis and Vitamin D. International journal of molecular sciences, 25(6), 3154.
- Bargiel, P.; Szczuko, M.; Stachowska, L.; Prowans, P.; Czapla, N.; Markowska, M.; Petriczko, J.; Kledzik, J.; J ˛edrzejczyk-Kledzik, A.; Palma, J.; et al. Microbiome Metabolites and Thyroid Dysfunction. J. Clin. Med. 2021, 10, 3609.