After a diagnosis of diverticulitis, diet becomes key in the remission of the affected patient. Here are the 3 essential factors addressed by the dietitian to prevent diverticulitis recurrences.
1. Promoting a high-fiber diet.
A diet rich in fiber, particularly cellulose, is associated with a reduced risk of diverticulitis. The literature is still uncertain about the exact amount to prioritize, but an intake of 20 to 35g - generally recommended for adults - is believed to be associated with a low risk of diverticular diseases. The two most plausible hypotheses regarding the mechanisms involved are related to the volume that fibers add to the stool, which accelerates intestinal transit, and the beneficial action of prebiotic fibers on the microbiota.
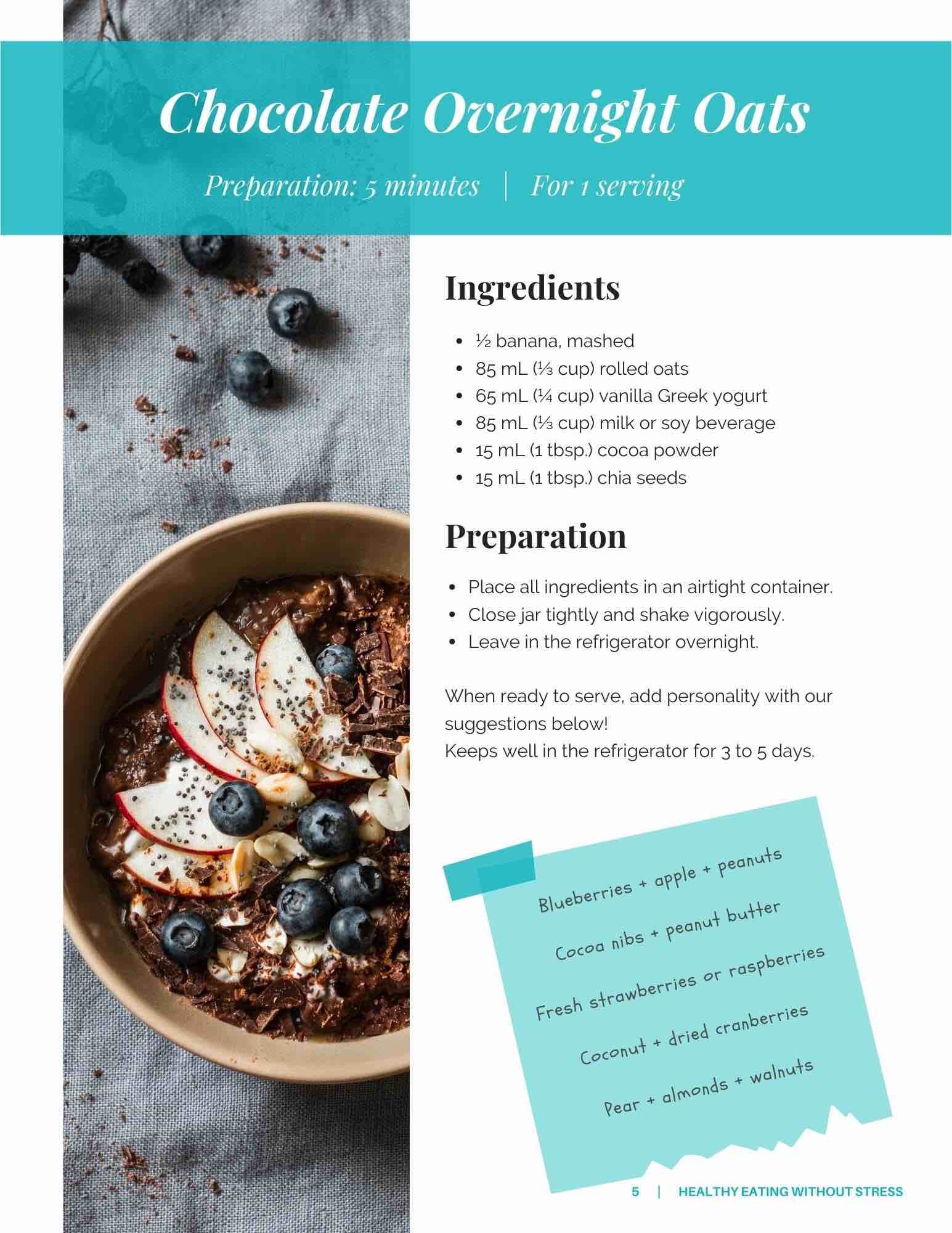
After a diverticulitis episode, patients are advised to gradually increase their fiber intake by 5g/day (or as tolerated), which can be determined with the dietitian. It can be as simple as choosing fiber-rich cereals (e.g., bran flakes) for breakfast, adding ½ cup of raspberries to yogurt for a snack, or swapping white pasta for whole wheat pasta for dinner.
Note: There is no need to avoid nuts, seeds, popcorn, and other foods containing seeds. Contrary to long-held beliefs, these foods do not increase the risk of diverticulitis.
2. Avoiding constipation.
Constipation is one of the major predictors of diverticulitis. There are many dietary changes that can promote good bowel movements, including reducing the consumption of processed foods (frozen meals, carbonated beverages, candies, chocolate, chips, etc.). These foods are typically low in fiber and provide little nutrition. Adequate hydration, at least 2.2 L/day for women and 3 L/day for men, helps reduce the risk of constipation.
Physical activity also helps maintain optimal bowel movements and is associated with a significant reduction in the risks of developing colonic diverticular disease and diverticulitis. A literature review has determined that being physically active can decrease the relative risk of diverticulitis by up to 24%. A similar association has been observed with weight: the higher the BMI, the higher the risks of diverticulitis.
3. Reducing red meat consumption.
The consumption of red meat, not chicken or fish, is strongly associated with an increased risk of diverticulitis. The mechanisms involved are not yet known, but several hypotheses exist. It is believed that metabolites resulting from the digestion of red meat could have an effect on the cells of the colon and promote the inflammation of diverticula. These metabolites may also alter the intestinal microbiota, influencing various parameters such as body weight.
Whether it is to maintain a healthy weight, reduce constipation, or increase fiber intake, a dietitian from Team Nutrition will accompany your patient following their diagnosis. They will ensure that the patient receives recommendations tailored to their risk factors, addressing their specific needs while keeping pleasure in mind.
References:
Carabotti M, Annibale B, Severi C, Lahner E. Role of fiber in symptomatic uncomplicated diverticular disease: a systematic review. Nutrients. 2017;9(2). Epub 2017/02/24. Crowe, FL et al. Diet and risk of diverticular disease in Oxford cohort of European Prospective Investigation into Cancer and Nutrition (EPIC): prospective study of British vegetarians and non-vegetarians. The British Medical Journal. 2011;343:d4131.
Aune D, Sen A, Leitzmann MF, Norat T, Tonstad S, Vatten LJ. Body mass index and physical activity and the risk of diverticular disease: a systematic review and meta-analysis of prospective studies. Eur J Nutr. 2017 Dec;56(8):2423-38.
* Image credit: People photo created by freepik - www.freepik.com