Published on May 28, 2024
Approximately 1 to 3% of the population is affected by histamine intolerance (1). This prevalence might be underestimated due to challenges associated with the availability of solid evidence concerning food intolerances, making evaluation and treatment difficult. Nonetheless, promising advancements are observed in the literature regarding the effectiveness of certain nutritional treatments for histamine intolerance.
Pathophysiology
This non-allergic food hypersensitivity is characterized by an imbalance between increased histamine availability and the capacity to adequately degrade this compound in the digestive system (2). Histamine is a biologically active amine produced by the body and primarily stored in basophils and mast cells, as well as in cells of the digestive system, lymph nodes, and thymus. It is involved in several essential bodily functions, such as immune response, digestion, and regulation of blood circulation. Normally, the enzyme histamine N-methyltransferase (HNMT) degrades histamine in the organs, while the comparatively small amount of histamine from external sources, such as from certain foods, is degraded by an enzyme primarily found in the small intestine and colon called diamine oxidase (DAO) (1).
Etiology and Symptoms
In individuals with histamine intolerance, insufficient activity of DAO and HNMT enzymes can be related to genetic factors (e.g., DAO enzyme mutation), medications (e.g., Metoclopramide, Amitriptyline, etc.), and alcohol. Additionally, inflammatory bowel diseases and gastrointestinal conditions that disrupt enterocyte cell integrity and intestinal flora can lead to histamine accumulation secondary to an imbalance between bacteria that produce (by decarboxylating the histidine amino acid precursor) and degrade histamine (with DAO enzyme) (2).
Symptoms of histamine intolerance vary considerably and may include digestive disorders such as bloating, diarrhea, headaches, fatigue, skin rashes like eczema, and allergy symptoms like rhinorrhea (2). These general manifestations differ from person to person and can be related to other food intolerances and medical conditions (e.g., irritable bowel syndrome), making diagnosis difficult. Due to the lack of consensus on a standard diagnostic method, there is no single test to determine histamine intolerance (3). Before making a diagnosis, the medical team must exclude other disorders or allergies that could cause similar symptoms. Histamine intolerance will be confirmed by combining skin tests for allergic reactions, blood tests to measure DAO levels, and a low-histamine diet to observe symptom improvement (2).
Nutritional Therapy
Exclusion Phase
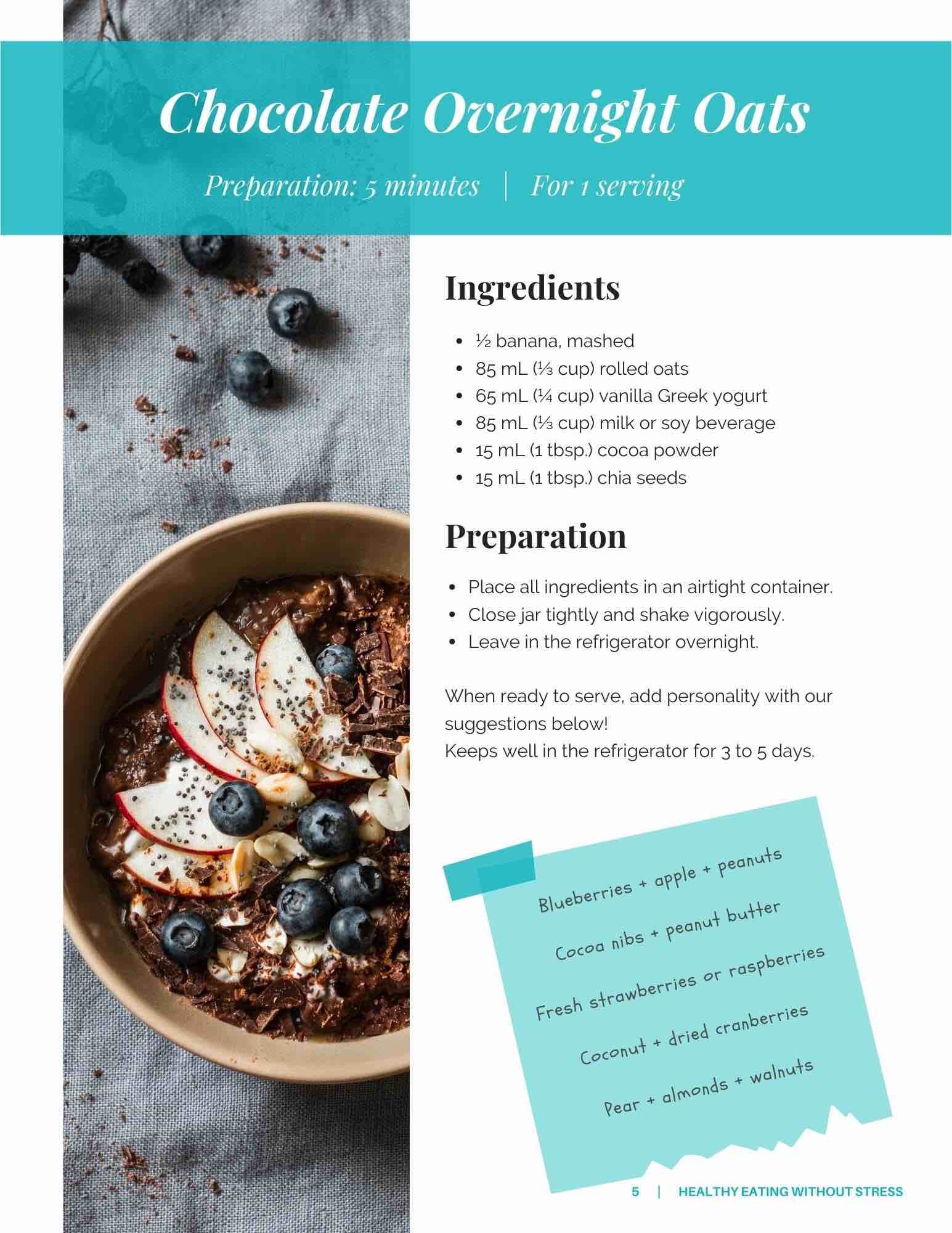
Nutritional therapy typically begins with an exclusion phase for 2 to 4 weeks. During this phase, histamine-rich foods are avoided, such as aged and fermented foods and beverages, certain fish, fruits, vegetables, and seasonings (4). Foods that may inhibit DAO enzyme function are also removed from the diet. Some examples of these include citrus fruits like grapefruit, alcoholic beverages, maté tea, and certain food additives (4).
Reintroduction Phase
After excluding certain foods, they are gradually reintroduced, one at a time, to identify specific triggers of symptoms. This approach allows for personalization of the diet, facilitating long-term management of the condition without compromising the patient-client's quality of life or nutritional diversity. This step should be done in collaboration with a nutritionist to identify foods to remove, find alternatives to these foods to avoid long-term nutritional deficiencies, and facilitate symptom management.
Supplementation
In addition to dietary adjustments, adding a DAO enzyme supplement may have positive effects by promoting the breakdown of ingested histamine. Several randomized controlled studies have reported reductions in gastrointestinal (5), cutaneous (5, 6), and migraine symptoms (5, 7) in individuals receiving enzymatic supplements.
Preventing Histamine Intolerance: Is It Possible?
More recently, some hypotheses have raised the association between histamine intolerance and intestinal permeability (4, 7) and/or intestinal dysbiosis (7, 8). Increased intestinal permeability caused by inflammation of the intestinal mucosa may allow more histamine and other irritant substances to cross the intestinal barrier, triggering allergic or adverse reactions in sensitive individuals. Dysbiosis can influence the balance of bacteria in the gut, leading to greater histamine production or reduced degradation. Although these two factors are not well established, some research suggests they could indirectly contribute to this intolerance. Two recent studies observed detrimental changes in the microbiota of patients with histamine intolerance symptoms. This dysbiosis was characterized by a decrease in bacteria associated with intestinal health and an increase in histamine-secreting bacteria (8, 9). Furthermore, a pilot clinical study evaluating changes in intestinal microbiota composition in participants diagnosed with histamine intolerance (n=5) following a nine-month dietary treatment observed improvements in gastrointestinal symptoms and headaches in some patients. This improvement was noted alongside an increased proportion of a bacterial group associated with improved intestinal health (10). These results suggest that managing gut flora health through diet and potentially a probiotic supplement (11, 12) could play a significant role in reducing the risk of developing histamine intolerance. A healthy diet is a major factor influencing the bacterial composition of the microbiota.
Histamine intolerance is a complex condition that requires a personalized approach for optimal management. At TeamNutrition, we are dedicated to providing personalized expertise and support for our patient-clients, enabling them to effectively manage this condition and improve their long-term intestinal health. For more information on managing histamine intolerance and to schedule an appointment with one of our specialists, visit our website or contact us directly.
References
- Maintz, L., & Novak, N. (2007). Histamine and histamine intolerance. The American journal of clinical nutrition, 85(5), 1185-1196.
- Comas-Basté, O., Sánchez-Pérez, S., Veciana-Nogués, M. T., Latorre-Moratalla, M., & Vidal-Carou, M. D. C. (2020). Histamine intolerance: The current state of the art. Biomolecules, 10(8), 1181.
- Jochum, C. (2024). Histamine Intolerance: Symptoms, Diagnosis, and Beyond. Nutrients, 16(8), 1219.
- Communauté d'intérêts Suisse de l'intolérance à l'histamine (SIGHI) (2023, 1 avril). Introduction. Récupéré le 21 mai 2024, sur https://www.mastzellaktivierung.info/fr/introduction.html
- Komericki, P., Klein, G., Reider, N., Hawranek, T., Strimitzer, T., Lang, R., ... & Aberer, W. (2011). Histamine intolerance: lack of reproducibility of single symptoms by oral provocation with histamine: a randomised, double-blind, placebo-controlled cross-over study. Wiener Klinische Wochenschrift, 123.
- Yacoub, M. R., Ramirez, G. A., Berti, A., Mercurio, G., Breda, D., Saporiti, N., ... & Colombo, G. (2018). Diamine oxidase supplementation in chronic spontaneous urticaria: A randomized, double-blind placebo-controlled study. International archives of allergy and immunology, 176(3-4), 268-271.
- Izquierdo-Casas, J., Comas-Basté, O., Latorre-Moratalla, M. L., Lorente-Gascón, M., Duelo, A., Soler-Singla, L., & Vidal-Carou, M. C. (2019). Diamine oxidase (DAO) supplement reduces headache in episodic migraine patients with DAO deficiency: A randomized double-blind trial. Clinical nutrition, 38(1), 152-158
- Schink, M., Konturek, P. C., Tietz, E., Dieterich, W., Pinzer, T. C., Wirtz, S., ... & Zopf, Y. (2018). Microbial patterns in patients with histamine intolerance. J Physiol Pharmacol, 69(4), 579-593.
- Sánchez-Pérez, S., Comas-Basté, O., Duelo, A., Veciana-Nogués, M. T., Berlanga, M., Latorre-Moratalla, M. L., & Vidal-Carou, M. C. (2022). Intestinal dysbiosis in patients with histamine intolerance. Nutrients, 14(9), 1774.
- Sánchez-Pérez, S., Comas-Basté, O., Duelo, A., Veciana-Nogués, M. T., Berlanga, M., Vidal-Carou, M. C., & Latorre-Moratalla, M. L. (2022). The dietary treatment of histamine intolerance reduces the abundance of some histamine-secreting bacteria of the gut microbiota in histamine intolerant women. A pilot study. Frontiers in Nutrition, 9, 1018463.
- Fiorani, M., Del Vecchio, L. E., Dargenio, P., Kaitsas, F., Rozera, T., Porcari, S., … Ianiro, G. (2023). Histamine-producing bacteria and their role in gastrointestinal disorders. Expert Review of Gastroenterology & Hepatology, 17(7), 709–718.
- Bischoff, S. C., Barbara, G., Buurman, W., Ockhuizen, T., Schulzke, J. D., Serino, M., Tilg, H., Watson, A., & Wells, J. M. (2014). Intestinal permeability--a new target for disease prevention and therapy. BMC gastroenterology, 14, 189.