The FODMAP-free diet is becoming increasingly popular for the treatment of irritable bowel syndrome (IBS) and many of your clients may ask you for your medical opinion on the subject. How does this diet work and what are the proven effects of it? Here is a short summary of the literature to help you understand the subject.
Mechanisms of action of the FODMAP-free diet
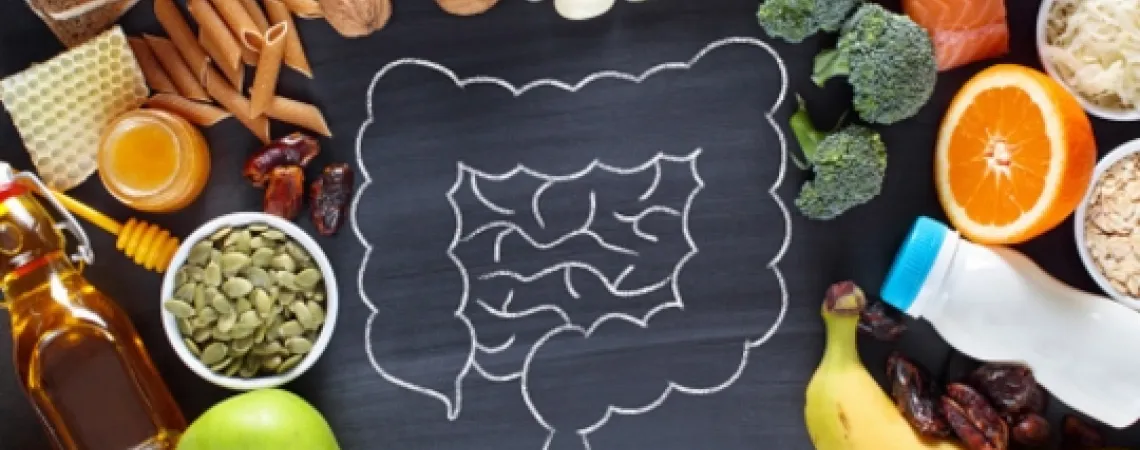
FODMAPs is an acronym for "Fermentable Oligosaccharides Disaccharides Monosaccharides And Polyols", which corresponds to different types of carbohydrates fermented by colonic bacteria that can cause symptoms such as bloating, abundant gas, discomfort and changes in stool consistency in IBS sufferers. Several mechanisms of action may explain this phenomenon, although most of them remain to be elucidated (1).
An increase in water in the intestinal lumen upon consumption of FODMAPs is well demonstrated, although how this phenomenon exacerbates the symptoms of people with IBS remains to be demonstrated (1). It has been suggested that this phenomenon can lead to pain and bloating for those with visceral hypersensitivity and contribute to loose stools and diarrhea (1). FODMAPs are also thought to increase the production of gases (hydrogen and methane) through fermentation (1,2). It would appear that visceral hypersensitivity to distension of the intestinal lumen caused by gas production seems to have more impact than distension itself, but further studies are needed (1). Other mechanisms have also been proposed, but the evidence is still limited: increased intestinal motility, a change in the gut microbiota, and a reduction in short-chain fatty acid production, which may play a role in visceral hypersensitivity and have several other impacts such as a change in gastrointestinal barrier permeability (1).
Finally, some small-scale or animal studies have also reported a decrease in the amount of histamine in the urine, normalization of colonic serotonin levels and stool lipopolysaccharide levels, and improvement in visceral hypersensitivity and intestinal mucosal integrity (3-5). Further studies are needed to elucidate these mechanisms.
What are the demonstrated effects of the FODMAP-free diet?
Compared to a traditional diet for the management of IBS, symptom improvement in 52% to 86% of patients has been reported in randomized controlled trials (2,6). According to a meta-analysis, a significant decrease in abdominal pain, bloating and overall symptoms is observed following a FODMAP-free diet in participants with IBS compared to a control group (7). These results are also observed in a systematic review, but the authors conclude that the evidence is limited due to the very low quality of the studies (8). Very few studies have observed the impact of a FODMAP-free diet in the long term (6). Moreover, the heterogeneity of these studies makes it difficult to interpret the results (6).
What is the suggested protocol?
The Canadian Association of Gastroenterology suggests that patients with IBS be offered a FODMAP-free diet for the shortest possible time (4 weeks) under the supervision of a nutritionist (9). The diet should consist of a restriction, reintroduction and customization phase (10). The restriction phase should include practical information (such as label reading, recipe adaptation and FODMAP-free recipe ideas) and alternative foods to increase adherence to the diet (10). The reintroduction phase helps to identify individual tolerance to each group of FODMAPs in order to improve dietary diversity and achieve nutritional adequacy (10). This phase is very important to avoid potentially negative impacts of the diet in the long term (see next paragraph). Personalization of the diet allows the diet to be tailored to control the symptoms of IBS, while coming as close as possible to a "normal" diet. This phase makes it possible to reach the recommendations in terms of macronutrients and micronutrients in order to avoid nutritional deficiencies as well as to ensure a pleasant diet and to reduce the impact on the patient's social life (10).
Are there potentially negative impacts of the FODMAP diet?
Conflicting results on the negative effects of the FODMAP-free diet are reported and explained by the methodological difference between studies as well as the lack of uniformity of recommendations between different countries (6). Among the important issues, an alteration of the microbiota is sometimes reported (6), including a decrease in Bifidobacteria and Faecalibacterium Prausnitzii, a bacterium of interest in gastrointestinal health (11). The potential impact on the risk of nutritional deficiencies is also an important issue, particularly with respect to calcium, thiamine, iron, carbohydrates, fiber, antioxidants and energy intake (1, 6). Conflicting results have been reported, but it is generally shown that the risk of deficiencies in these micronutrients or macronutrients is low when the client is supervised by a nutritionist (1,2,6).
The nutritionist: an essential expert in accompanying the client in this process.
The support of a qualified nutritionist is very important in order to explain the objective and the nature of the diet to the patient, to avoid energy imbalances or dietary deficiencies and to ensure adherence through regular monitoring and adaptation of the diet to individual preferences and lifestyle (6). A TeamNutrition Nutritionist will be able to guide your patients through these steps. Do not hesitate to contact us for more information on our services!
References:
- Staudacher HM et Whelan K. The low FODMAP diet: recent advances in understanding its mechanisms and efficacy in IBS.Gut. 2017;66(8):1517-1527.
- Liu J, Chey WD, Haller E et al. Low-FODMAP Diet for Irritable Bowel Syndrome: What We Know and What We Have Yet to Learn. Annu Rev Med. 2020;71:303-314.
- Mazzawi T, Hausken T, Gundersen D et al. Dietary guidance normalizes large intestinal endocrine cell densities in patients with irritable bowel syndrome. Eur J Clin Nutr 2016;70:175–181.
- Zhou SY, Gillilland M, Wu X et al. FODMAP diet modulates visceral nociception by lipopolysaccharide-mediated intestinal inflammation and barrier dysfunction. J Clin Invest. 2018;128(1):267-280.
- McIntosh K, Reed DE, Schneider T et al. 2016. FODMAPs alter symptoms and the metabolome of patients with IBS: a randomised controlled trial. Gut 66(7):1241–1251.
- Bellini M, Tonarelli S, Nagy AG et al. Low FODMAP Diet: Evidence, Doubts, and Hopes. Nutrients. 2020;12(1):148.
- Marsh A, Eslick EM et Eslick GD. Does a diet low in FODMAPs reduce symptoms associated with functional gastrointestinal disorders? A comprehensive systematic review and meta-analysis. Eur J Nutr. 2016;55(3):897-906.
- Dionne J, Ford AC, Yuan Y et al. A Systematic Review and Meta-Analysis Evaluating the Efficacy of a Gluten-Free Diet and a Low FODMAPs Diet in Treating Symptoms of Irritable Bowel Syndrome. Am J Gastroenterol. 2018;113(9):1290-1300.
- Moayyedi P, Andrews CN, MacQueen G et al. Canadian Association of Gastroenterology Clinical Practice Guideline for the Management of Irritable Bowel Syndrome (IBS). J Can Assoc Gastroenterol. 2019;2(1):6-29.
- Whelan K, Martin LD, Staudacher HM et al. The low FODMAP diet in the management of irritable bowel syndrome: an evidence-based review of FODMAP restriction, reintroduction and personalisation in clinical practice. J Hum Nutr Diet. 2018;31(2):239-255.
- Lopez-Siles M, Ducan SH, Jesus Garcia-Gil L et al. Faecalibacterium prausnitzii: from microbiology to diagnostics and prognostics. ISME J. 2017;11(4):841-852.